Liver Cancer
Liver Cancer
What Is Liver Cancer?
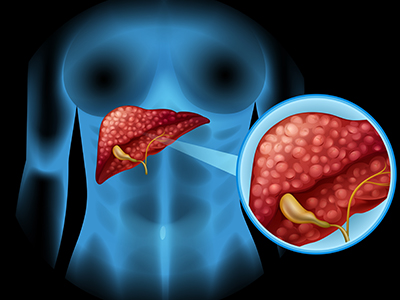
The liver is a vital organ responsible for filtering blood from the digestive tract, synthesizing essential proteins and chemicals for various bodily functions, including clotting, metabolism, digestion, and drug detoxification.
Liver cancer, medically known as hepatocellular cancer, originates within the liver. It can develop from abnormal cell growth within the liver, which may lead to issues like internal bleeding or bile duct blockages. Early detection is key to effectively treating liver cancer, although it can be challenging to diagnose as symptoms often manifest in advanced stages.
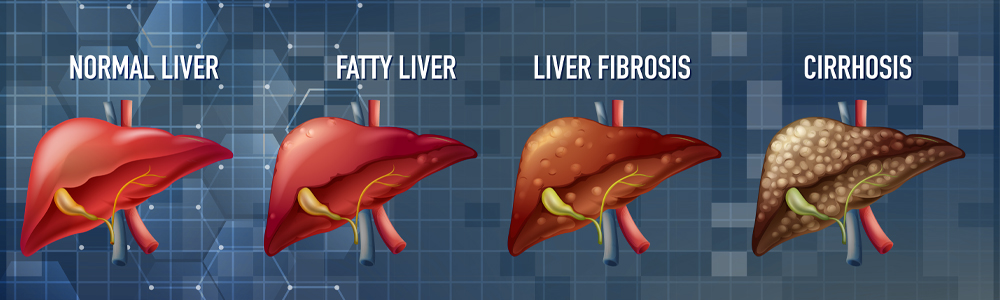
Liver cancer encompasses a range of cancers affecting the liver. It may be categorized as primary liver cancer, which originates within the liver itself, or secondary/metastatic cancer, which spreads from other parts of the body to the liver. Primary liver cancer often results from liver damage due to factors like cirrhosis, alcohol abuse, certain birth defects, chronic infections (such as hepatitis B and C), hemochromatosis, obesity, fatty liver disease, and more.
Types Of Liver Cancer
Liver cancer originates in an essential organ responsible for many vital bodily functions. It can be broadly classified into five distinct types, each affecting the liver in its unique way. These various liver cancer types are all serious and tend to have a recurring nature. The different categories of liver cancer include:
Hepatoblastoma is a form of liver cancer typically found in children. Early detection of this cancer is associated with a 90% survival rate, surpassing many other cancer types. In its initial stages, hepatoblastoma is curable, and treatments can significantly improve the overall life expectancy of young cancer patients.
Hepatocellular carcinoma (HCC) is a common primary liver cancer, frequently affecting individuals with pre-existing liver damage. It can originate at multiple sites within the liver or as a single tumor. The development of this cancer is initiated when hepatocyte cells sustain damage and subsequently exhibit uncontrolled growth.
These fast-growing liver cancers commence within the blood vessels inside the liver. Unfortunately, their diagnosis is typically achievable only in advanced stages.
While this disease is considered rare, it has shown greater treatment effectiveness against liver cancer when compared to other types of the disease.
This type originates in the bile duct, a small tube that carries bile to the gallbladder. These tumors are often greenish in color, but they can also appear yellowish and have a rubbery consistency.
The liver is essential for life, as it performs a vast number of biochemical reactions on a daily basis. Liver tumors can be benign or malignant. Some common benign tumors are:
- Cysts
- Fibroma
- Lipoma
- Leiomyoma
- Hemangioma
- Hepatic adenoma
- Focal nodular hyperplasia
Signs And Symptoms Of Liver Cancer
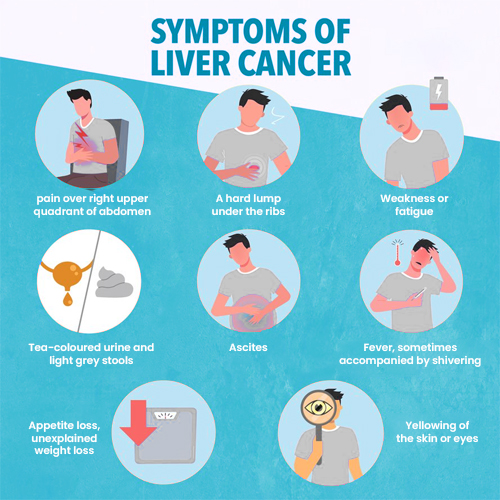
The liver cancer symptoms can be difficult to detect at first. The patient may feel nothing or only mild discomfort. Initially, the patient might not realize that they have liver cancer. But as it spreads, some of these symptoms are bound to appear:
- Fatigue
- Jaundice
- Vomiting
- Fever
- Itching
- An enlarged liver
- Loss of appetite
- Unexplained weight loss
- Swelling or fluid build-up in the abdominal area
- Change of skin color and the change of eye white part to yellow
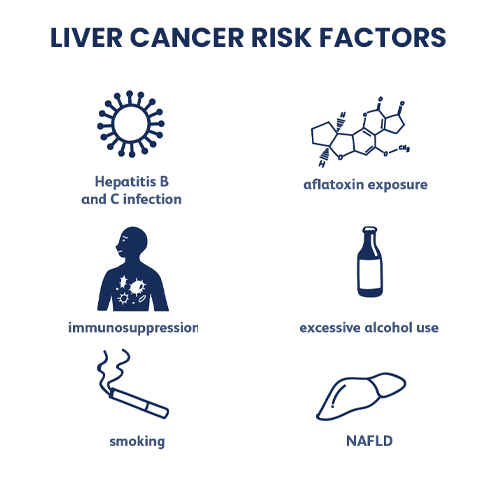
Causes And Risk Factors Related To Liver Cancer
There are chances of infection in the liver, jaundice, and hepatitis that may result in cancer if not treated properly and completely. By knowing it and understanding the causes, you can try to avoid these risks. There are a few reasons that trigger the risks related to liver cancers:
The symptoms of liver cancer can be challenging to detect initially. Patients may experience no symptoms or only mild discomfort. They might not initially realize they have liver cancer. However, as the disease progresses, some of these symptoms may emerge:
1. DNA mutations in liver cells can lead to the disease.
2. Rapid growth of tumor cells.
3. Conditions like diabetes may increase the risk of liver disorders.
4. Infections from hepatitis viruses, such as Hepatitis A and B.
5. Conditions like Wilson’s disease and hemochromatosis can contribute to liver infections.
6. Alcoholism is a major risk factor for the development of liver cancer.
7. Liver cirrhosis can result from the scarring of liver cells and may lead to liver cancer.
8. Contaminated food with aflatoxins can cause liver disorders and infections that may progress to liver cancer.
9. Nonalcoholic fatty liver disease, characterized by excessive fat accumulation in the liver, increases the risk of liver cancer.
Diagnosis Of Liver Cancer
Liver cancer is diagnosed through a series of screening tests. The doctor may recommend liver function tests to identify potential causes of tumor cell growth. A physical examination is conducted to look for symptoms or lumps that might suggest the presence of liver cancer. Additionally, several other tests may be performed to diagnose liver cancer, such as:
– Imaging studies like ultrasound, CT scans, and MRI scans to visualize the liver and any tumors.
– A liver biopsy, where a sample of liver tissue is taken for laboratory analysis.
– Blood tests to check for tumor markers or other abnormal blood components.
– A laparoscopy, which allows direct examination of the liver through a thin, flexible tube with a camera.
– Exploratory surgery to visually inspect the liver and surrounding areas for cancer.
In this procedure, high-frequency sound waves are directed into the body.
Through this test, detailed images of the organs are provided.
It is the injection of a dye that is done into an artery that shows tumors and liver tissues.
In this test, a computer, a large magnet, and radio waves are produced that provide clear images of the human body.
A laparoscope is a thin tube with a light, camera, and lens at one end. It is used for looking inside the abdomen. The doctors can see everything through this tube. This instrument is also used in various procedures including the removal of tumors or biopsies (taking small pieces of tissue out for examination under a microscope).
In order to adequately monitor the progress of the treatment and ensure a positive outcome, blood tests are performed for several parameters. The tests also include liver enzymes and serum marker tests. The measurement of some substances associated with cancer can be done by performing a serum marker test. An underlying liver problem is indicated with the help of liver enzymes.
Stages Of Liver Cancer
Barcelona Clinic Liver Cancer (BCLC) staging system is a cancer staging system for the liver that is used to classify cancers by their extent and whether they have spread to other parts of the body. The stages of liver cancer include:
- Stage 0
- Stage 1
- Stage 2
- Stage 3
- Stage 4
It is known as the very early stage.
It is called the early stage where the tumor is only seen in the liver. This is further classified into two stages:
- Stage 1A: A single tumor that is not larger than 2 centimeters (a little less than an inch), which has not advanced into the blood vessels or spread to lymph nodes or distant sites.
- Stage 1B:A solitary tumor whose size is more than 2 cm and has not advanced into the blood vessels. Even no spread to lymph nodes or distant sites is noticed.
Here in this stage of cancer the one tumor present could spread to blood vessels. Even one more tumor which is about 5cm can also be present.
In the third stage, only one tumor bigger than 5cm is noticed. There is a probability that cancer has moved beyond the liver to lymph nodes, blood vessels, or to another organ. It has two stages:
- Stage 3A:More than one tumor is seen where one is about 5cm and no spread is seen to lymph nodes or distant sites.
- Stage 3B:One or more tumors of any size may be present with at least one advanced into the portal vein or hepatic artery. No spread to lymph nodes or distant sites is noticed.
In this stage, cancer has spread to different body parts such as bones or lungs along with lymph nodes or distant sites. It also has two more stages including:
- Stage 4A: Cancer has spread to lymph nodes but has not spread to distant sites.
- Stage 4B: The disease at this stage is spread to body parts including bones or lungs. The spread may or may not be seen in lymph nodes.
Treatment Options For Liver Cancer

The treatment of liver cancer is a complex and long-term process that involves both surgical and non-surgical procedures. The choice of treatment depends on factors such as the type of cancer, its stage, the patient’s age, and gender. Liver cancers detected in the early stages can often be treated with surgery to prevent the disease from progressing and potentially leading to fatal outcomes.
Liver Cancer Treatment Options
- Liver Transplant
- Non-transplant
- Chemotherapy
- Radiotherapy
- Percutaneous Ethanol Injection
A liver transplant is a complex surgical procedure that involves replacing a diseased liver with a healthy one from a donor. This option is considered when the patient's liver is no longer functioning properly and has not responded to other medical treatments. There are two main types of liver transplants:
1. Deceased Donor Liver Transplantation (DDLT): DDLT involves replacing the patient's diseased liver with a healthy liver obtained from a recently deceased donor. Patients must undergo a series of tests to determine their eligibility for a transplant and are then placed on a waiting list until a suitable donor liver becomes available.
2. Living Donor Liver Transplantation (LDLT): In this procedure, a portion of a healthy liver from a living donor, often a family member or friend, is transplanted into the patient with the diseased liver. The transplanted liver segment has the capacity to regenerate and grow to its normal size. LDLT is typically chosen when the patient requires an urgent transplant, and a deceased donor liver transplant is not a viable option.
The treatment of liver cancer includes two main procedures:
1. Radiofrequency Ablation (RFA): RFA is a non-transplant surgical option that is used to eliminate cancerous cells. This minimally invasive procedure involves the use of image guidance to insert a needle through the skin and into the liver tumor. A high-frequency electrical current is then passed through the needle, creating heat that destroys the cancer cells. RFA has proven to be highly effective in treating liver diseases and is recommended when surgery is not a viable option.
2. Partial Hepatectomy: This surgical procedure is commonly employed to remove liver cancer or cirrhosis. It involves the removal of a portion of the liver, which can range from a smaller section to an entire lobe, depending on the extent of the disease.
Chemoembolization (TACE - Trans Arterial Chemoembolization) of the hepatic artery is a medical procedure that involves blocking the artery to deprive a liver tumor of blood and nutrients, ultimately leading to its destruction. This treatment can be employed either as a standalone therapy or in combination with other treatments such as radiotherapy, surgery, or radiation therapy, depending on the specific needs and condition of the patient.
TARE (Transarterial Radioembolization), EBRT (External Beam Radiotherapy), and SBRT (Stereotactic Body Radiation Therapy) are various treatment options that can be considered for the management of certain cancer cases. These treatments employ radiation to target and treat cancer cells effectively. TARE specifically uses tiny radioactive beads that are inserted into blood vessels to irradiate the tumor, while EBRT and SBRT deliver radiation from outside the body to precisely target the cancer. The choice of treatment depends on the type and stage of cancer, as well as the individual patient's condition.
Percutaneous ethanol injection (PEI) is indeed a medical procedure used in the treatment of certain liver cancers, including hepatocellular carcinoma (HCC), which is the most common form of primary liver cancer. During PEI, ethanol (alcohol) is injected directly into the tumor within the liver. The ethanol dehydrates and damages the cancer cells, leading to changes in their structure and protein denaturation. This procedure can be effective in treating specific cases of liver cancer, particularly in patients who are not candidates for surgery or liver transplantation. However, its suitability depends on the extent and location of the tumor and the overall health of the patient.
Follow Up After Liver Cancer Treatment
A follow-up examination is a routine medical check-up with your physician to monitor your health status. It may involve physical examinations, medical tests, or a combination of both. During these visits, your doctor will assess whether there are any treatment-related side effects and ensure that you are recovering as expected. It’s important to communicate any changes or concerns you experience with your doctor to facilitate appropriate follow-up care.
To aid in your recovery and overall well-being, here are some helpful tips:
1. Allow yourself sufficient rest and self-care.
2. Give your body time to heal after treatment.
3. Engage in social activities to boost your spirits.
4. Avoid taking on strenuous tasks at work or home.
5. Incorporate regular, moderate exercise into your routine.
6. Promptly consult your physician if you experience any discomfort.
7. Adopt a balanced diet rich in green vegetables while minimizing junk food consumption.
The type of cancer, its stage, whether cancer has spread, and your overall health all influence treatment options. The goal of treatment is to eliminate as many malignant cells as possible while minimizing damage to neighboring healthy cells. This is made feasible by technological advancements.
Follow Up After Liver Cancer Treatment
Selecting the right hospital for liver cancer treatment is crucial, as it significantly impacts one’s life and health. When making your choice, consider factors like the hospital’s reputation, medical equipment, and the expertise of its healthcare professionals. Here are some top hospitals renowned for their liver cancer treatment services:
1. Aster Medcity, Kochi
2. HCG Manavata, Nashik
3. Fortis BG Road, Bengaluru
4. Kokilaben Ambani Hospital
5. Fortis Hospital, Vadapalani
6. Fortis C-DOC, Chirag Enclave
7. Manipal Hospital, Whitefield
8. Fortis La Femme, Greater Kailash
9. Manipal Hospital, Old Airport Road
10. BKL Superspeciality Hospital, New Delhi
11. Fortis Escorts Heart Institute, Okhla Road
Remember to conduct thorough research and consult with healthcare professionals to make an informed decision about the most suitable hospital for your liver cancer treatment.
FAQs
The rate at which cancer spreads can vary depending on the type of cancer and individual factors. Hemangiosarcomas and angiosarcomas are indeed known to be aggressive cancers that can spread rapidly. On the other hand, hepatocellular carcinoma (a primary liver cancer) may have a different growth rate and pattern of spread. However, the exact speed and extent of cancer spread can be influenced by various factors, including the stage at diagnosis, treatment options, and the patient’s overall health. It’s essential to discuss these specifics with a healthcare provider when dealing with a cancer diagnosis.
Liver cancer presents a significant challenge to cure, with primary liver cancer often remaining undetectable during its most treatable stages. Secondary liver cancer, which has spread, can be particularly challenging to treat. In cases where a cure is not possible, doctors may opt for palliative treatment to manage symptoms and improve the patient’s quality of life.
In most cases, traditional chemotherapy is not the preferred option for treating liver cancer. Instead, doctors often recommend a different form of chemotherapy known as hepatic artery infusion (HAI).
Yes, it is possible to cure liver cancer with non-surgical methods such as Radiofrequency Ablation and Partial Hepatectomy.
When liver cancer cell grows into the nearby lymph nodes, they spread easily to other parts of the body by lymphatic circulation.
Prevention is indeed better than cure, and there are several measures individuals can take to reduce the risk of liver cancer, including:
1. Getting vaccinated for Hepatitis B.
2. Practicing safe sex and avoiding intravenous drug use to prevent Hepatitis C.
3. Using sterilized needles for piercing and tattooing.
4. Consuming alcohol in moderation.
5. Maintaining a healthy weight through a balanced diet and regular exercise.
6. Limiting exposure to cancer-causing chemicals in the environment.
In this procedure, the entire liver is removed and replaced with another healthy liver from an organ donor. In most cases, a suitable healthy liver can be found within 24 hours of the surgery.
Some of the tests include a physical examination and medical history, serum tumor marker test, liver function test, CT scan, and MRI. A biopsy is typically performed in conjunction with laparoscopy to confirm the diagnosis.
Oftentimes, it is possible to cure cancer if it is detected early. Regular health screenings can help detect liver cirrhosis and viral hepatitis early. An integrated approach involving a multidisciplinary team is the best way to successfully combat liver cancer.
If you are experiencing any side effects of the treatment, it’s essential to inform your doctor immediately so that a follow-up treatment plan can be properly designed and maintained.

At MediTours India, we stand as a distinguished leader in the realm of medical tourism, dedicated to transforming your healthcare journey into a seamless and transformative experience. With a commitment to excellence and a focus on your well-being, we pave the way for a new era of medical travel.
Contact Us
Address : C603 Jalaram Park LBS Road. Bhandup West Mumbai -400078 Phone : +91 9820344697 Email : ajit@meditoursindia.in
Copyright by indiameditours 2023. All rights reserved.